Tips for a Safer Mind amid the Pandemic. Mental health matters

 Covid-19 Drive through testing in Kigali City Entry Point.
Covid-19 Drive through testing in Kigali City Entry Point.
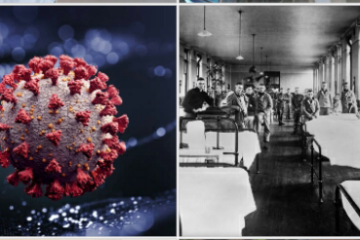
It’s been almost nine months since the outbreak of the ongoing world pandemic of COVID-19 which first broke out in Wuhan, China in December 2019. The World Health Organisation currently reports 17.5 million COVID-19 cases with more than 680, 000 deaths as said by the WHO Director-General, Dr. Tedros in his opening remarks to the media on 3rd August 2020. Well, all this has brought great attention to general medical complications associated with the COVID-19. However, this has slightly left behind another important aspect called “Mental health” which is why I would like to take this opportunity to discuss the mental health disorders (psychological well-being), their risk factors and what we can do to handle the risk factors thus enabling us to copy up with reality. My major objective in this article is comfort all of us who have been drained psychologically, just to show them that they are not alone. We are in this together. Among these disorders are panic disorder, anxiety, depression, post traumatic stress disorder (PTSD), Prolonged grief disorder and other mental disorders associated with COVID -19. I’ve divided this article into two parts where part 1 will tackle the causes and risk factors and finally part 2 where I tackle some of the measures to help us handle and deal with these challenges effectively.
Part 1: Risk factors
Well, it is of no surprise that natural disasters of which COVID-19 happens to be the case that induce alot of mind challenging effects such as losing a parent or a loved one with saying or kissing him or her goodbye. Scientists are relentlessly working on the vaccines but it looks we have to work ways to contain the virus for a while. So, in this section, am working to raise awareness on the major factors that tend to deteriorate our mental health as far as the pandemic is still ongoing.
Recent research has showed that the deaths resulting from COVID-19 are making it harder for the bereaved to copy up with the pandemic which leads to a mental health disorder known as prolonged grief disorder which as long as six months and beyond.
There has also been the work from home programs for places which are still under lock down and quarantine thereby making it hard for parents to copy with the situation since most of them are working with their kids around, making it hard to be productive. On the other side, here comes homeschooling which makes it hard for parents especially due to lack of sufficient educational resources.
The fear of contracting the virus itself is also mind blowing on the side of health individuals.
Research has also showed that the health care providers especially the front liners who are directly involved in COVID-19 treatment are not able to sleep enough either due to lack of enough time or stress.
With most people, lock down which has left most services closed has caused temporary unemployment which is mind draining.
Another research has found guilt in some bereaved individuals in which most of them feel like they did not do enough for their deceased which also a mind deteriorating factor.
Isolation is also another mind deteriorating factor since the people experiencing such psychology effects are most healed through social interaction with friends, family and mainly the psychiatrists by use of “talking therapy” which can’t easily be accessed.
Part 2: measures
As a reversal, just like matter which has it’s antagonist as anti-matter, likewise there are some helpful strategies that one can use to fight those mind blowing risk factors and stay positive in such times where the pandemic is uttermost. But hold on, before going any further, I would like to appreciate the psychiatrists who working relentlessly to help us keep our minds at ease by use of other alternatives such as setting up online sites to help their patients as a way of limiting the chances of being exposed to the virus. Among others include telemedicine and other alternatives being implemented but basically is that I am aware of their efforts such as the WHO, the American Psychological Association (APA), ..etc. Well, the following are some of the tips to help you handle these risk factors:
First things first, currently, the flow of information and misinformation about the pandemic is heavy that it requires one to choose reliable sources such as the WHO, CDC, Health ministries and health professionals. This way, it will help you keep calm.
Take care of your body through exercising regularly, trying to eat healthy, getting enough sleep, etc.
Consider the problem-solving recommendations against the virus in your daily activities. This will enable you reduce the worry of getting infected. Among these recommendations are wearing a face mask that covers your mouth and nose, washing and sanitising your hands, social distancing.
Structure your day and create an atmosphere/space that will enable you perform your daily duties efficiently.
Connect and keep in touch with friends, family and colleagues. For these people matter alot and will help you keep calm as for we, humans are social animals.
Taking breaks from reading, watching and listening to whatever stories that we engage.
Knowing what to do of your are sick with COVID-19 and contacting a health professional before starting any self treatment.
Well, as for now, I hope I have tackled the essentials on mental health as far as the pandemic is concerned and therefore it is about us to be aware of such factors that expose us to mental health disorders. In addition to that, this will enable us seek a timely treatment thereby mitigating another epidemic from happening.
Bibliography :
- Klein, Alice. “Grief over covid-19 deaths may be unusually severe and long-lasting.” Last modified July 8, 2020. https://www.newscientist.com/article/2248095-grief-over-covid-19-deaths-may-be-unusually-severe-and-long-lasting/
- WHO DIRECTOR-GENERAL. “WHO Director-General’s opening remarks at the media briefing on COVID-19 – 3 August 2020.” Last modified August 3, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—3-august-2020
- Vindegaad, Nina., Eriksen, M. “COVID-19 pandemic and mental health consequences: Systematic review of the current evidence.” Last modified May 16, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7260522/
- Sélim, B.Guessoum., Jonathan, L., Marie, R. “Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown.” Last modified June 29, 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7323662/
- Sanwang, Wang., Minghu, C. “Psychological Influence of Coronovirus Disease 2019 (COVID-19) Pandemic on the General Public, Medical Workers, and Patients With Mental Disorders and its Countermeasures” Last modified May 22, 2020. https://www.sciencedirect.com/science/article/pii/S0033318220301432
- WHO. “Mental health & COVID-19. https://www.who.int/teams/mental-health-and-substance-use/covid-19
- CDC. “Coping with Stress.” Last modified July 1, 2020. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html

0 Comments